Are Some Humans Immune To Coronavirus – The novel coronavirus is newly emergent in humans. Therefore, the general population is susceptible because they lack immunity against it. 2019-nCoV can infect individuals with normal or compromised immunity. The amount of exposure to the virus also determines whether you get infected or not.
If you are exposed to a large amount of virus, you may get sick even if your immune function is normal. For people with poor immune function, such as the elderly, pregnant women or people with liver or kidney dysfunction, the disease progresses relatively quickly and the symptoms are more severe.
The dominant factor determining whether one gets infected or not is the chance of exposure. So, it cannot be simply concluded that better immunity will lower one’s risk of being infected.
Children have fewer chances of exposure and thus a lower probability of infection. However, at the same exposure, senior people, people with chronic diseases or compromised immunity are more likely to get infected.
What are the epidemiological characteristics of COVID-19?
The emergent epidemic of COVID-19 has experienced three stages: local outbreak, community communication, and widespread stage (epidemic).
Transmission dynamics: in the early stage of the epidemic, the average incubation period was 5.2 days; the doubling time of the epidemic was 7.4 days, i.e., the number of people infected doubled every 7.4 days; the average continuous interval (the average interval time of transmission from one person to another) was 7.5 days; the basic regeneration index (R0) was estimated to be 2.2 to 3.8, meaning that each patient infects 2.2 to 3.8 people on average.
As for the main average intervals — for mild cases, the average interval from onset to the initial hospital visit was 5.8 days, and that from onset to hospitalization 12.5 days; for severe cases, the average interval from onset to hospitalization was 7 days and that from onset to diagnosis 8 days; for fatality cases, the average interval from onset to diagnosis was significantly longer (9 days), and that from onset to death was 9.5 days.
The COVID-19 epidemic passed three stages of communication: 1) the stage of local outbreak (cases of this stage are mostly related to the exposure of a seafood market); 2) the stage of community communication (interpersonal communication and clustering transmission in communities and families); 3) widespread stage (rapid spread, with large population flow, to the entire country of China and even the world.)
What are the routes of transmission of 2019-nCoV?
At present, it is believed that transmission through respiratory droplets and contacts is the main routes, but there is a risk of fecal-oral transmission. Aerosol transmission, mother to child transmission and other routes are not confirmed yet.
Respiratory droplet transmission is the main mode of direct contact transmission. The virus is transmitted through the droplets generated when patients are coughing, sneezing or talking, and susceptible persons may get infected after inhalation of the droplets.
The virus can be transmitted through indirect contacts with an infected person. The droplets containing the virus are deposited on the surface of the object, which may be touched by the hand. The virus from the contaminated hand may get passed to the mucosa (or mucosae) of oral cavity, nose and eyes of the person and lead to infection.
The live novel coronavirus has been detected from feces of confirmed patients, suggesting the possibility of fecal-oral transmission.
RELATED: Coronavirus Thrives On Hard Flat Surfaces
When the droplets are suspended in the air and lose water, pathogens left behind to form the core of the droplets (i.e. aerosols). Aerosols can fly to a distance, causing long-distance transmission. This mode of transmission is called aerosol transmission. There is no evidence that the novel coronavirus can be transmitted through aerosol yet.
A child of the mother with COVID-19 was confirmed to have positive throat swabs after 30 hours of birth. This suggests that the novel coronavirus may cause neonatal infection through mother to child transmission, but more scientific research is in need to confirm this route.
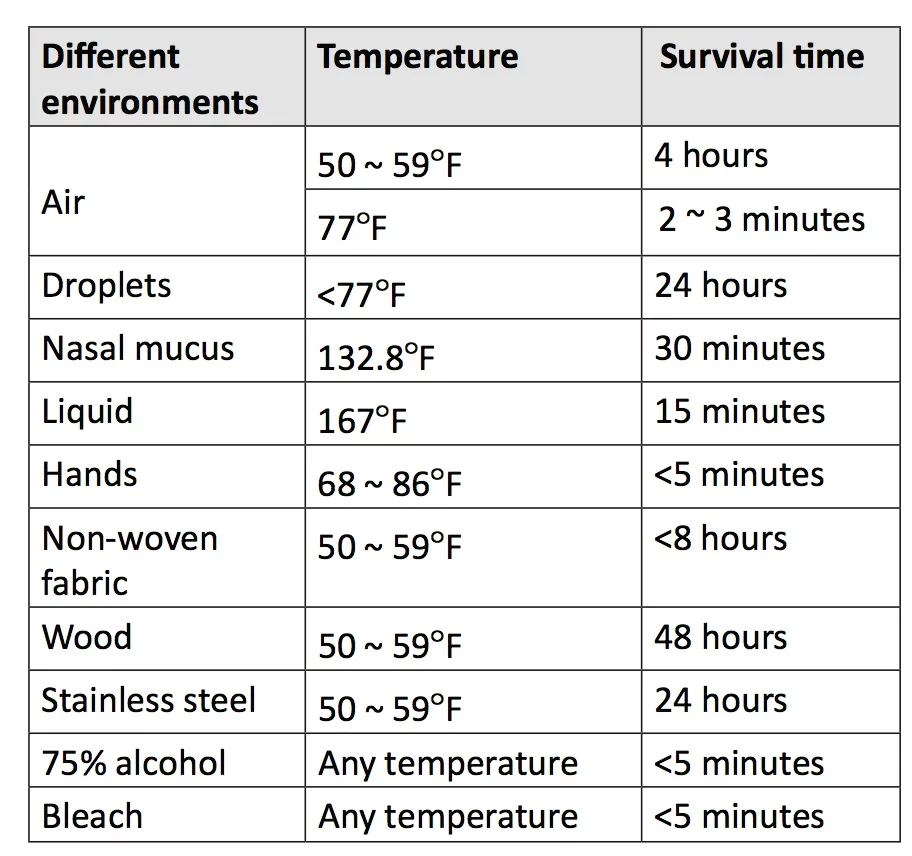
How resilient are coronaviruses in different environments?
Viruses generally can survive for several hours on smooth surfaces. If the temperature and humidity permit, they can survive for several days. The novel coronavirus is sensitive to ultraviolet rays and heat.
Sustained heat at 132.8° F for 30 minutes, 75% alcohol, chlorine-containing disinfectants, peracetic acid, chloroform, and other lipid solvents can effectively inactivate the virus. Chlorhexidine (also known as chlorhexidine gluconate) also efectively inactivates the virus.
Common coronaviruses mainly infect adults or older children, causing the common cold. Some strains can cause diarrhea in adults. These viruses are mainly transmitted by droplets, and can also be spread via the fecal-oral route. The incidence of corona virus infection is prevalent in winter and spring. The incubation period for coronaviruses is usually 3 to 7 days.
The survival time of the novel coronavirus at different environmental temperatures is as follows:
2019-nCoV is a coronavirus that underwent genetic mutations. The incubation period of the virus is as short as 1 day but generally considered to be no longer than 14 days. But it should be noted that some reported cases had an incubation period of up to 24 days.
Can humans develop immunity to 2019-nCoV?
Scientific data on the level and the duration of protective immune antibodies produced in patients after infection of the novel coronavirus remain scarce.
In general, the protective antibodies (immunoglobulin G, IgG) against a virus can be produced two weeks or so after an infection, and may exist for several weeks to many years, preventing re-infection of the same virus after recovery. Currently efforts are underway to test whether recently those recovered from 2019-nCoV infection carry protective antibodies in the blood.
How do I prevent COVID-19 infection in cinemas and theaters?
During an epidemic outbreak, try to avoid visits to public spaces, especially places with large crowds and poor ventilation (like cinemas). Wear a face mask if visits to public spaces are required. Cough or sneeze into tissues completely covering the nose and mouth.
Seal used tissues in a plastic bag before discarding immediately in a closed bin labeled “residual waste” or “medical waste” to prevent the virus from spreading. Operators of public spaces should maintain a hygienic indoor environment, ensure regular ventilation and sterilization every day.
What about on public transit?
Passengers on public transport such as bus, metro, ferry or planes must wear face masks to reduce the risk of getting infected in crowded spaces. Seal used tissues in a plastic bag before discarding immediately in a closed bin labeled “residual waste” or “medical waste” to prevent the virus from spreading.
Are elevators a risk?
Yes. An elevator carries a high risk of transmission due to its confined space. To prevent the spread of 2019-nCoV in elevators, the following measures should be taken:
(1) The elevator should be thoroughly and regularly disinfected several times with ultraviolet irradiation, 75% alcohol or chlorine-containing disinfectants every day.
(2) Minimize the risks of getting infected from sneezing by taking the elevators alone if possible.
(3) Wear a mask before entering the elevator. If someone sneezes in the elevator while you have no masks on, cover your mouth and nose with your sleeves. Measures like clothes-changing and personal cleaning should be taken right after.